How did the infected blood scandal affect Scotland?
 Getty Images
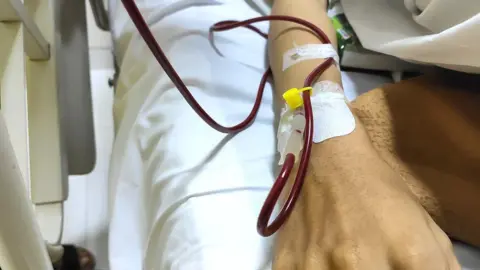
Getty ImagesA public inquiry into the contaminated blood scandal of the 1970s and 1980s is publishing its final report.
More than 30,000 people in the UK were infected with HIV and Hepatitis C after being given NHS blood products. Thousands of them were in Scotland.
Sir Brian Langstaff’s inquiry examined the whole of the UK - but there were some key differences in how the scandal unfolded on opposite sides of the border.
What happened in Scotland?
It is estimated that about 3,000 people in Scotland were given infected blood in the 1970s and 80s.
Many had received blood transfusions on the NHS, while others were being treated for haemophilia.
Hundreds have now died.
One area where Scotland differed from the rest of the UK is that the vast majority of infections came from its own blood donations.
In the 1970s and 80s, the country was largely self-sufficient in blood products.
In addition to having adequate local donations for the population’s needs, the Protein Fractionation Centre in Edinburgh had the capacity to process blood plasma to manufacture treatments for haemophilia or certain forms of immune deficiencies.
 PA Media
PA MediaUnlike other parts of the UK, there was no need to rely on commercial products from America.
The Scottish National Blood Transfusion Service (SNBTS) has been criticised for not adequately screening donors and for taking donations from prisoners.
With a higher population of intravenous drug users, prisoners were known to be at greater risk of infection.
The SNBTS continued this practice as late as March 1984, a year after England stopped and two years after warnings from the Medicines Inspectorate.
There were also delays to the introduction of screening for hepatitis C that could have prevented some infections.
The head of the Scottish National Blood Transfusion Service apologised to the victims ahead of the publication of the report.
Children's hospital used US supplies
Although most of the blood used in Scotland was from Scottish donations, the exception was Yorkhill hospital in Glasgow where children were treated for haemophilia.
They regularly received plasma products sourced from paid donors in the United States that were known to be high risk.
Most of the children were infected with HIV or hepatitis C by the age of five.
Some went on to develop AIDS.
Their families want to know why clinicians chose American products ahead of Scottish blood and why there were delays to the introduction of heat treatment.
Scotland’s public inquiry
Scotland was the first part of the UK to commission a public inquiry into infected blood.
It had been a key election pledge of the SNP government when it came to power in 2007, and was carried out by Scottish judge Lord Penrose.
But the Penrose inquiry lacked the full statutory powers to compel witnesses from outside of Scotland to give evidence, and until 1999 health policy had been controlled by Westminster.
In the end, after six years of investigation at a cost of about £12m, the report made just one recommendation - that anybody who had a blood transfusion before 1991 should be screened for hepatitis C.
Its publication in 2015 was condemned as a "whitewash" by many of those affected. Some set fire to copies of it in the street.
Campaigner Bill Wright said the publication of the report had been a disappointment, but added that it had led to "better things” in Scotland.
"We developed a better support scheme than had existed in the rest of the UK and there was a tiny wee light at the end of the tunnel,” he said.
The UK-wide inquiry was announced in 2017 after years of campaigning by victims. Led by former judge Sir Brian Langstaff, it took evidence between 2019 and 2023.